What is the recommended frequency and duration of electrocardiogram monitoring in patients receiving intravenous haloperidol?
Background
Haloperidol is a first-generation antipsychotic (FGA) that nonselectively blocks postsynaptic dopaminergic (D2) receptors in the brain, although its full mechanism of action is unknown.1-3 Depending on the dosage form, the drug is approved for second-line treatment of behavioral disorders and hyperactivity in children, schizophrenia in adults and children, and management of tics in Tourette syndrome in adults and children. Haloperidol also has numerous off-label indications, including delirium, nausea and vomiting, and severe, acute agitation or aggression outside of the approved populations. Haloperidol is available as an oral tablet, oral solution, and intramuscular injection. The intramuscular injection is supplied as a decanoate and lactate formulation. The decanoate formulation cannot be administered by intravenous (IV) route due to its sesame oil preparation and insolubility in water..4 However, data supporting IV administration of the lactate formulation are available.1-3,5 Depending on the indication for use, the recommended dose of IV haloperidol via bolus injection is 0.5 to 20 mg; IV infusion is used less frequently, with a dose range between 0.5 to 35 mg/hour reported in the literature.
While IV administration of haloperidol is commonly done in practice, there is concern for cardiac events with administration of the drug by this route.6,7 Notably, in 2007, the Food and Drug Administration (FDA) mandated a stronger warning be added to the haloperidol prescribing information with regard to the increased risk of QT interval prolongation and torsades de pointes (TdP) with IV administration or higher than recommended doses of any formulation.7
Cardiac risk with IV haloperidol
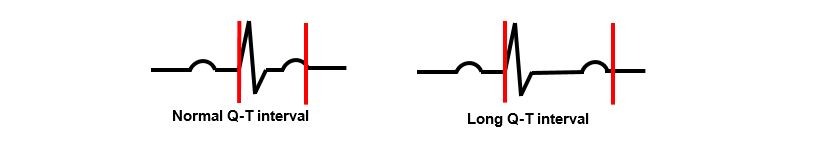
Prolongation of the QT interval has been reported with haloperidol use, and high doses and/or IV administration appear to increase risk.8,9 A prolonged QT interval is due to delayed cardiac repolarization and can increase the risk of ventricular tachyarrhythmia, including TdP, and sudden death (Figure 1).
Risk factors for haloperidol‐associated QT interval prolongation and TdP were evaluated in a systematic review.7 In this review, TdP and/or QT interval prolongation generally occurred in patients with concomitant risk factors for QT interval prolongation (underlying cardiac disease, electrolyte imbalance, etc) and in those administered cumulative doses ≥2 mg. A summary of risk factors for QT prolongation and TdP are found in Table 1.10
Table 1. Risk factors for QT interval prolongation and TdP.10 Heading link
| Table 1. Risk factors for QT interval prolongation and TdP.10 | |
|---|---|
| Drug-related | Other |
| Antiarrhythmics: amiodarone, sotalol | Older age |
| Antibiotics: azithromycin, ciprofloxacin, levofloxacin, erythromycin, moxifloxacin | Female gender |
| Antidepressants: citalopram, escitalopram | Heart disease |
| Antiemetic: ondansetron | Arrhythmias |
| Antifungal: fluconazole | Renal or hepatic impairment |
| Antipsychotic: haloperidol | Genetic predisposition to QT prolongation |
| Opiate: methadone | Electrolyte abnormalities (hypokalemia and hypomagnesemia) |
| Abbreviations: TdP= Torsades de Pointes. | |
The length of the QT interval is dependent on the heart rate; a shortened interval occurs in the presence of tachycardia whereas bradycardia lengthens the interval.8 To compare QT intervals over time, a “corrected” interval (generally noted as QTc) is calculated and provides an estimate of the QT interval at a heart rate of 60 beats per minute. There are 4 correction calculators for QT interval measurements: Bazett, Fridericia, Framingham, and Hodges.8 While not a consistently reliable method of correcting the QT interval for heart rate, Bazett’s formula is programmed into most electrocardiogram (ECG) machines for clinical use. Normal and at-risk values for QT interval measurements are based on this formula (see Table 2).
Table 2. Bazett-corrected QT interval measurements.8 Heading link
| Table 2. Bazett-corrected QT interval measurements.8 | ||
|---|---|---|
| Rating | Adult Men (ms) | Adult Women (ms) |
| Normal | < 430 | < 450 |
| Borderline | 431 to 470 | 451 to 480 |
| Prolonged | > 470 | > 480 |
| Abbreviations: ms=milliseconds. | ||
Best practices for ECG monitoring
Recommendations for ECG monitoring in patients receiving IV haloperidol are not standardized and generally driven by institutional policies and procedures.7,8 However, because patient-specific comorbidities and other risk factors for QT interval prolongation may confound the association between IV haloperidol and the development of TdP, there is uncertainty whether ECG monitoring is clinically useful for all patients who are administered this therapy.7-10 The remainder of this review summarizes ECG monitoring recommendations from various sources for patients receiving IV haloperidol.
Tertiary sources
Haloperidol is listed on crediblemeds.com as having a “known risk of TdP.”11 Tertiary drug information databases, including Lexicomp, Micromedex, and Clinical Pharmacology, in accordance with the prescribing information for haloperidol, recommend ECG monitoring if the agent is administered by IV route.1-3, 6 Micromedex and Lexicomp specifically recommend an ECG at baseline.1,2 Lexicomp also recommends continuous ECG monitoring if the patient has risk factors for QT prolongation, has a prolonged QT interval at baseline, or is receiving cumulative IV doses that are ≥2 mg.2
Guidelines
Two national organizations present slightly conflicting recommendations for ECG monitoring in patients receiving antipsychotics with associated cardiac risks (see Table 3).8,10 A 2018 American Psychiatric Association (APA) resource document on QT prolongation and psychotropic medications recommends obtaining an ECG no more than 1 month prior to initiation of an antipsychotic that may increase the risk of TdP.8 Monitoring for any changes in medications, electrolytes, and cardiovascular status (ie, acute myocardial infarction or heart failure) should also occur around the time of initiating the drug. However, this document explains that the absence of a baseline QT interval should not prevent the prescribing of antipsychotic medications that may increase the risk of TdP if the benefits outweigh the risks. Per the APA, clinicians should be proficient in the measurement, calculation, and documentation of the QT interval. Unfortunately, recommendations for the frequency of ECG monitoring are not discussed in this document.
For hospitalized patients, the 2017 American Heart Association (AHA) update to practice standards for ECG monitoring in the hospital setting does not recommend QT monitoring for all patients that start antipsychotics or nonantiarrhythmic drugs with known risk for TdP.10 Notably, QT monitoring is not recommended for patients without a history of prolonged QT or risk factors for TdP who are started on nonantiarrhythmic drugs with known, possible, or conditional risk for TdP. The AHA backs their recommendation by stating that nonantiarrhythmic drugs with known, possible, or conditional risk for TdP, including antipsychotic agents, are generally initiated in the outpatient setting without ECG monitoring. Additional recommendations from the AHA are provided in Table 3.
Table 3. Recommendations for ECG monitoring in patients taking antipsychotics.8,10 Heading link
| Table 3. Recommendations for ECG monitoring in patients taking antipsychotics.8,10 | |
|---|---|
| Organization | Recommendations |
| American Heart Association, 2017 | QT interval monitoring is recommended for:
QT interval monitoring is reasonable for:
QT interval monitoring is not recommended for:
General principles
|
| American Psychiatric Association, 2018 | A QT interval measurement should be done no more than 1 month prior to initiation of an antipsychotic that may increase the risk of TdP. |
Primary literature
Adherence to the FDA’s warning for ECG monitoring with IV haloperidol use has been inconsistent across practice sites and settings.7,12-14 In a 2017 single-center, cross-sectional survey (N=52 physicians at all training levels) aimed at characterizing trends in ECG monitoring practices before initiation of antipsychotics, over 50% of the respondents did not screen for history of syncope, prolonged QT, family history of sudden death, or electrolyte abnormalities; more than half of respondents did, however, screen for heart disease and arrhythmias.12 In the same survey, physicians were more likely to order ECGs before initiation of antipsychotics in the inpatient vs outpatient settings; however the proportion of respondents ordering ECGs during significant dose titrations in the presence of cardiac risk factors was approximately 50% in both setting. When asked about which resources respondents consulted to guide their decisions on cardiac monitoring, most respondents relied on current literature or residency training over outdated guidelines. Overall, this study demonstrates that cardiac risk stratification is important to most providers and guides monitoring decisions with regards to ECGs. Limitations of this survey include a low response rate (55%) and lack of detail on the practice setting for certain questions.
An older single-center, retrospective, cohort study (N=556) assessing practices for ECG monitoring of elderly patients receiving IV haloperidol found that over 3 years, 58% of patients receiving the drug did not receive cardiac monitoring in accordance with expert recommendations available at the time.13 In this study, adherence to expert recommendations included all of the following: completion of an ECG within 7 days of the first dose of IV haloperidol, avoidance of IV haloperidol if the baseline QT is ≥500 ms, and ECG within 24 hours of the first dose of haloperidol if the baseline QT was ≥450 ms. Notably, 20% of patients did not have a baseline ECG, and more than 1 in 10 elderly patients with a QT of greater than 500 ms received the drug. Limitations of this study include its retrospective nature and outcomes based on a single, first dose of IV haloperidol. The study authors propose the use of customized alerts or decision support using computerized physician order entry (CPOE) in order to improve provider adherence to ECG monitoring recommendations in patients receiving IV haloperidol. Interestingly, a 2012 retrospective, pre- and post-implementation study did see an increase in the performance of baseline and follow up ECGs in patients receiving IV haloperidol after implementation of an IV haloperidol CPOE order set.14 The order set in this study called for ECG monitoring within 24 hours of administration of IV haloperidol; if multiple doses were given in a short period of time, an ECG was needed within 24 hours of the last dose.
Overall, the literature seems to support ECG monitoring in patients receiving IV haloperidol in cases where there are known risk factors for QT prolongation and TdP. As previously noted, telemetry for QT interval monitoring may be overused in patients receiving IV haloperidol who do not have risk factors for TdP or only require low doses of IV haloperidol. As demonstrated in other studies, while the use of telemetry outside of critical care units does not usually result in major therapeutic changes, unnecessary ECG monitoring may also result in unnecessary testing and treatment, and higher cost of care.15,16
Recommendations
There is not a consensus on which patients receiving IV haloperidol should also receive ECG monitoring or how often such monitoring should occur. However, based on a review of information from the manufacturer, tertiary drug databases, and the primary literature, the following practices are consistently noted:
- A baseline QT interval should be obtained ≤1 month before initiation of IV haloperidol in patients with risk factors for QT interval prolongation or TdP or a history of prolonged QT interval.
- The QT interval should be monitored during therapy in patients with risk factors for QT prolongation or TdP or a history of prolonged QT; the recommended frequency of such monitoring is unclear, but ranges from every 8 to 24 hours across references.
- In the absence of risk factors for QT prolongation or TdP, ECG monitoring is likely not needed for patients receiving cumulative IV haloperidol doses of <2 mg/day.
- If the baseline QT interval is ≥500 ms, IV haloperidol should be avoided.
References
- Micromedex Solutions [database online]. Greenwood Village, CO: Truven Health Analytics, Inc; 2019. http://www.micromedexsolutions.com/. Accessed December 17, 2019.
- Lexicomp [database online]. Riverwoods, IL: Wolters Kluwer Health, Inc; 2019. http://www.online.lexi.com/. Accessed December 17, 2019.
- Clinical Pharmacology [database online]. Tampa, FL: Gold Standard, Inc; 2019. https://www.clinicalkey.com/pharmacology/. Accessed December 17, 2019.
- Park EJ, Amatya S, Kim MS, et al. Long-acting injectable formulations of antipsychotic drugs for the treatment of schizophrenia. Arch Pharm Res. 2013;36(6):651-659.
- Riker RR, Fraser GL, Cox PM. Continuous infusion of haloperidol controls agitation in critically ill patients. Crit Care Med. 1994;22(3):433-440.
- Haldol [package insert]. Titusville, NJ: Janssen Pharmaceuticals; 2019.
- Meyer-Massetti C, Cheng CM, Sharpe BA, et al. The FDA extended warning for intravenous haloperidol and torsades de pointes: how should institutions respond? J Hosp Med. 2010;5(4):E8-16.
- Funk MC, Beach SR, Bostwick JR, et al. Resource document on QT prolongation and psychotropic medications. American Psychiatric Association https://www.psychiatry.org/psychiatrists/search-directories-databases/library-and-archive/resource-documents. Updated June 2018. Accessed December 17, 2019.
- Beach SR, Celano CM, Sugrue AM, et al. QT prolongation, torsades de pointes, and psychotropic medications: a 5-Year update. Psychosomatics. 2018;59(2):105-122.
- Sandau KE, Funk M, Auerbach A, et al. Update to practice standards for electrocardiographic monitoring in hospital settings: a scientific statement from the american heart association. Circulation. 2017;136(19):e273-e344.
- Drugs that prolong QT & induce Torsades de Pointes (TdP). CredibleMeds website. https://crediblemeds.org/index.php/drugsearch. Accessed December 17, 2019.
- Broszko M, Stanciu CN. Survey of EKG monitoring practices: a necessity or prolonged nuisance? Am J Psych. 2017;12(3):6-9.
- Chueng D, Wolfe B. Unsafe use of intravenous haloperidol: evaluation of recommendation-concordant care in hospitalized elderly patients. J Am Geriatr Soc. 2013;61(1):160-161
- Muzyk AJ, Rivelli SK, Jiang W, et al. A computerized physician order entry set designed to improve safety of intravenous haloperidol utilization: a retrospective study in agitated hospitalized patients. Drug Saf. 2012;35(9):725-31.
- Sivaram CA, Summers JH, Ahmed N. Telemetry outside critical care units: patterns of utilization and influence on management decisions. Clin Cardiol. 1998;21(7):503-505.
- Henriques-Forsythe MN, Ivonye CC, Jamched U, et al. Is telemetry overused? Is it as helpful as thought? Cleve Clin J Med. 2009;76(6):368-372.
- J. Muzyk, A. Rayfield, J.Y. Revollo, et al. Examination of baseline risk factors for QT interval prolongation in patients prescribed intravenous haloperidol. Drug Saf. 2012;35(7):547-553.
Prepared by:
Jasmine Mangrum, PharmD, MPH
PGY1 Pharmacy Practice Resident
College of Pharmacy
University of Illinois at Chicago
Reviewed by:
Katherine Sarna, PharmD, BCPS
Clinical Assistant Professor
College of Pharmacy
University of Illinois at Chicago
January 2020
The information presented is current as of November 15, 2019. This information is intended as an educational piece and should not be used as the sole source for clinical decision making.